
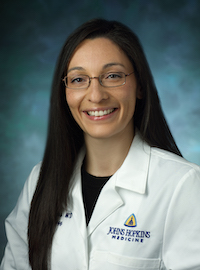
Lisa McElroy, MD, MS
CHART Scientific Director
Abdominal Transplant Surgeon
Assistant Professor of Surgery
Assistant Professor of Population Health Sciences
Duke University School of Medicine
lisa.mcelroy@duke.edu
Lisa M McElroy, MD, MS, is an Assistant Professor of Surgery and Population Health Sciences at Duke University and the Onyekwere E. Akwari Assistant Professor of Surgery. She is the Director of Health Services Research for the Duke Department of Surgery.
Dr. McElroy’s research examines the influence of organizational characteristics on clinical outcomes of high cost, high acuity patients. Her current projects, which aim to improve equity in access to transplantation by reducing bias in processes of care, are funded by the Robert Wood Johnson Foundation, the American Surgical Association and the National Institutes of Health. She is an Associate Editor of the American Journal of Transplantation.

Allan D. Kirk, MD, PhD
Abdominal Transplant Surgeon
Chair, Duke University Department of Surgery
Surgeon in Chief, Duke Health
allan.kirk@duke.edu
Allan D. Kirk, MD, PhD, FACS, is chair of the Department of Surgery in the Duke University School of Medicine and Surgeon-in-Chief for Duke University Health System. He is the David C. Sabiston, Jr. Distinguished Professor of Surgery and a professor of immunology and pediatrics.
Dr. Kirk directs the Laboratory of Immune Management in the Department of Surgery at Duke University School of Medicine. His research focuses on the following three interrelated areas: 1) the use of costimulation blockade therapy to prevent organ rejection in transplant recipients, 2) antibody depletion therapies to condition patient immune systems for transplant, and 3) understanding how immunosuppressive agents can affect the immune system based on immune exhaustion, memory, and senescence.
Dr. Kirk is internationally recognized for work in transplant immunology, serving as the inaugural Chief of the Transplantation Branch for the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and principal investigator for multiple clinical trials, including the first-in-man experience with novel immunosuppressive agents. He served as Editor-in-Chief for the American Journal of Transplantation from 2010 through 2020 and is now Editor Emeritus.
Duke Data Coordinating Center Team

Ursula Rogers
Senior Informaticist
Duke Department of Sugery
ursula.rogers@duke.edu

Roland A. Matsouaka, PhD
Assistant Professor of Biostatistics & Bioinformatics
Duke Department of Biostatistics & Bioinformatics
roland.matsouaka@duke.edu

Tyler Schappe, MS
Biostatistician
Duke Department of Biostatistics & Bioinformatics
tyler.schappe@duke.edu

Andrew Olson, MPP
Associate Director, Strategy and Solutions for Health Data Science
Duke AI Health
andrew.olson@duke.edu
Samuel I. Berchuck, PhD
Assistant Professor of Biostatistics & Bioinformatics
Duke University School of Medicine
sib2@duke.edu

Jennifer A. Gagnon, BS, RN
Director of Healthcare Analytics and Innovation
Duke University Department of Surgery
jennifer.gagnon@duke.edu
Participating Institutions


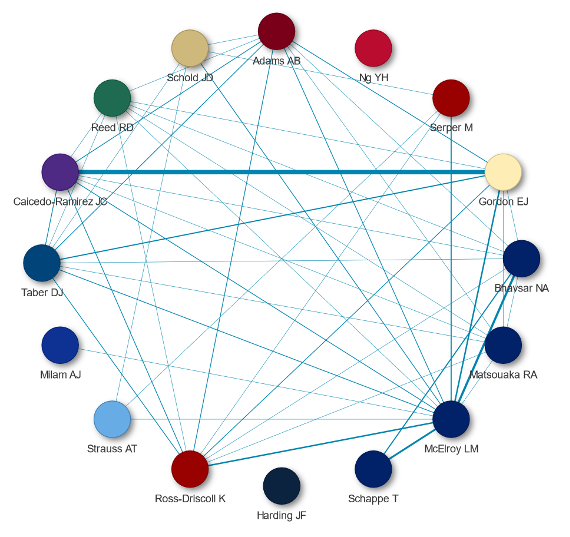

Andrew Adams, MD, PhD
Abdominal Transplant Surgeon and Professor of Surgery
Director, Solid Organ Transplant Service Line
University of Minnesota
adam1717@umn.edu
Andrew Adams, MD, PhD is a Professor and the John S. Najarian Surgical Chair in Clinical Transplantation in the Department of Surgery at the University of Minnesota Medical School. He is also the Executive Medical Director for the Solid Organ Transplant Service Line at M Health Fairview. Dr. Adams earned his medical degree from Emory University Medical School, before completing his residency at Harvard Medical School and Massachusetts General Hospital. He returned to Emory University following residency to complete a transplant fellowship and later joined their faculty. There, he established an innovative translational research lab focused on developing cutting-edge technologies that improve patient care and outcomes for transplant patients.
As a transplant surgeon and scientist, Dr. Adams is interested in developing the best therapies and diagnostics for transplant patients by understanding the fundamental mechanisms of the immune system that give rise to organ rejection. As a graduate student, under the direction of Drs. Chris Larsen and Tom Pearson, Dr. Adams investigated the efficacy of costimulation blockade and helped develop Belatacept, now a clinically available therapy for transplant patients. Belatacept leads to improved survival and kidney function for renal transplant patients. The Adams’ Lab has four main areas of investigation: 1) costimulation blockade and costimulation independent rejection, 2) xenotransplantation, 3) transplant diagnostics, 4) transplant outcomes.
Dr. Adams' research efforts are concentrated on the development of novel strategies and therapeutics to promote transplantation tolerance. He has made important contributions to our understanding concerning the interplay between viral infection, immune memory, and the allo-immune response. Dr. Adams is also an internationally recognized expert in large animal models of xenotransplantation.

Katherine Ross-Driscoll, PhD, MPH
Assistant Professor
Division of Transplantation
Department of Surgery
Indiana University School of Medicine
krossdr@iu.edu
Katherine Ross-Driscoll, PhD, MPH is an Assistant Professor in the Department of Surgery at Indiana University School of Medicine. Dr. Ross-Driscoll was previously an Assistant Professor of Surgery at Emory University, and was a member of the Emory Transplant Health Services and Outcomes Research Program of the Department of Surgery, as well as the Health Services Research Center at Emory. She earned her Master of Public Health and PhD, both in Epidemiology, at the Rollins School of Public Health at Emory University.
Her primary research focuses on the influence that access to care and quality of care has on racial, socioeconomic, and geographic disparities in outcomes among patients with end-stage liver disease (ESLD). Dr. Ross-Driscoll has been building a diverse body of work in health services research since her MPH years, has received a variety of research awards including the Young Innovator Award and the Young Investigator Award from the American Society of Transplant Surgeons, and been published in such leading journals as the American Journal of Transplantation, Transplantation, and the Journal of the American Medical Association.

Jessica Harding, PhD
Epidemiologist and Assistant Professor in the Department of Surgery
Emory University
jessica.harding@emory.edu
Dr. Jessica Harding is an epidemiologist with extensive experience in conducting chronic disease research at population and system levels in both academic and government settings.
She received her PhD in medical research (epidemiology) from Baker Heart and Diabetes Institute, Melbourne, Australia, in 2016, and engaged in a research fellowship at the Centers for Disease Control and Prevention from 2017-2019. During the latter period she focused on describing trends in diabetes and kidney disease-related complications in the United States, and examined variations in diabetes incidence and diabetes complications according to demographic, socioeconomic, and lifestyle risk factors.
At Emory, Dr. Harding is working on improving data collection and quality related to kidney disease and transplantation as a member of the Transplant Health Services and Outcomes Research Program.

David J. Taber, PharmD, BCPS
Transplant Pharmacist and Associate Professor of Surgery
Director of Transplant Clinical Trials
Medical University of South Carolina
taberd@musc.edu
David J. Taber, Pharm.D., BCPS is an Associate Professor of Surgery and the Director of Transplant Clinical Trials at the Medical University of South Carolina College of Medicine. Dr. Taber earned both his Pharm.D. and his Master of Science in Public Health from MUSC. He completed a post-doctorate pharmacy specialty residency in transplantation at The University of North Carolina at Chapel Hill. Dr. Taber has approximately 15 years of post-residency experience providing pharmaceutical care to transplant patients.
Dr. Taber’s current research endeavors surround the study of optimizing medication utilization in transplantation and studying mechanisms to improve the peri-operative value of care in transplant surgery. He was recently the PI of a R18 study with the U.S. Department of Health & Human Services, Agency for Healthcare Research and Quality (AHRQ). The primary purpose of the Transplant Medication Safety through a Pharmacist-Empowered, Patient-Centered, mHealth-Based Intervention (TRANSAFE Rx) study was to demonstrate significant reductions in medication safety issues leading to reduced healthcare resource utilization in kidney transplantation through a pharmacist-led, mHealth-enabled intervention. Dr. Taber was recognized by his peers as the recipient of the 2017 Distinguished Investigator Award by the American College of Clinical Pharmacists.

Vineeta Kumar, MD
Professor of Medicine
Robert and Curtessa Bourge Endowed Professor in Transplant Nephrology
University of Alabama
kumarv@uab.edu
Vineeta Kumar, MD, is a Professor of Medicine and the Robert and Curtessa Bourge Endowed Professor in Transplant Nephrology at the University of Alabama in Birmingham, where she serves as lead nephrologist for the Living Kidney Donor and Incompatible Kidney Transplant programs.
She is an expert in kidney transplantation, living kidney donation, incompatible kidney transplantation, kidney paired donation, and cardiovascular outcomes after kidney transplantation.

Peter Reese, MD, PhD
Professor of Surgery, Biostatistics, and Medicine
Director, Vanderbilt Center for Transplant Science
peter.reese@vumc.org
Peter Reese, MD, PhD, is a transplant nephrologist and epidemiologist. His research focuses on: a) developing effective strategies to increase access to kidney transplantation, b) improving the process of selecting and caring for live kidney donors, c) determining outcomes of health policies on vulnerable populations with renal disease, including the elderly, and d) testing strategies to improve important health behaviors such as medication adherence. He was a co-founder of Penn’s Center for Quality, Analytics and Research in Transplantation (PQART). He is past Chair of the Ethics Committee for the United Network for Organ Sharing (UNOS), which oversees organ allocation and transplant regulation in the United States. In recognition of his contributions to transplant research, he received a Presidential Early Career Award for Scientists and Engineers (PECASE) in July 2012. The PECASE "recognizes and supports scientists and engineers who show exceptional promise for leadership at the frontiers of scientific knowledge."
In the transplant field, Dr. Reese and his colleagues pioneered the practice of transplanting organs from donors with hepatitis C virus infection into uninfected recipients. He has written specifically about the ethical implications of accepting live kidney donors with risk factors for kidney disease, live donor outcomes, the effects of organ allocation policy on vulnerable subgroups including children and the elderly, and better policy strategies to promote the careful use of higher-risk organs.
Dr. Reese’s mission encompasses energetic support of talented and motivated young researchers at all stages of training. This Lab’s success reflects their creativity and efforts. Currently our research group includes individuals with diverse content interests, including solid organ transplantation, health behavior change, obesity, social networks as well as methodological interests in advanced multivariable matching and causal modeling. We benefit from multiple members with NIH K grants, several who now run their own independent research programs, and others at every stage of training. Their publications, awards, promotions and the new knowledge they create are a credit to their efforts.
He is also a practicing transplant nephrologist at Vanderbilt University Medical Center.

Juan C. Caicedo-Ramirez, MD
Abdominal Transplant Surgeon and Professor of Surgery
Director of the Hispanic Kidney Transplant Program
Northwestern University
j-caicedo@northwestern.edu
Juan C. Caicedo Ramirez, MD is a Professor of Surgery at Northwestern University Feinberg School of Medicine, where he also serves as the Director of the Hispanic Kidney Transplant Program. Dr. Caicedo is Director of the Liver Transplant Program, Living Donor Liver Program, and Hispanic Transplant Program at Northwestern Medicine. He is an adult and pediatric transplant surgeon who is actively involved in the adult kidney and liver transplant programs, including the living donor program for both kidney and liver. Dr. Caicedo is also involved in hepatobiliary surgery and advanced laparoscopic procedures. His primary goal has been to increase living kidney and liver donation and transplantation for Hispanic patients using a culturally competent and congruent approach that has been very successful. Dr. Caicedo has been a Co-Principal Investigator on a NIH funded grant to disseminate and implement his Hispanic Transplant Program. He receives calls from transplant centers around the world seeking his advice on how to replicate the model in their own institutions.
Aly T. Strauss MD, PhD, MIE
Assistant Professor of Medicine
Co-Director of the Clinical and Translational Research Unit for Gastroenterology and Hepatology
Johns Hopkins University
astraus6@jhmi.edu
Aly Strauss is an Assistant Professor of Medicine at Johns Hopkins University School of Medicine, where she also serves as the Co-Director of the Clinical and Translational Research Unit for the Division of Gastroenterology and Hepatology. She is an adult hepatologist who cares for general hepatology patients as well as pre- and post-liver transplant patients.
Dr. Strauss is currently funded by the NIH on a K08 to study the use of data science for improving health equity for patients referred for liver transplantation. Previously, Dr. Strauss completed her Masters in Industrial Engineering at the University of South Florida and her PhD in Clinical Investigation at the Johns Hopkins Bloomberg School of Public Health. She is a faculty member in the Johns Hopkins University Malone Center for Engineering in Healthcare.
Lastly, Dr. Strauss serves as an editorial board member for Liver Transplantation, a member on the Lesbian, Gay, Bi-sexual, Transgender, Queer (LGBTQ) Task Force for the American Association for the Study of Liver Diseases (AASLD), a member on the American Society for Gastrointestinal Endoscopy (ASGE) Diversity and Inclusion Committee, and a member on the Quality Committee for the American Gastroenterology Association (AGA).

Yue-Harn Ng, MD
Clinical Associate Professor
Director, Transplant Fellowship Program
Division of Nephrology
University of Washington
yharn1@uw.edu
Dr. Yue-Harn Ng received her medical degree from McGill University, Faculty of Medicine, in Montreal, Canada. She completed her Internal Medicine residency, Nephrology and Transplant Nephrology Fellowship at the University of Pittsburgh.
Dr. Ng has over 15 years of clinical experience caring for kidney transplant patients. She joined the Division of Nephrology at the University of Washington in 2020 as an Associate Professor of Medicine. She currently also holds the title of Transplant Nephrology Fellowship Program Director.
Dr. Ng is the Diversity, Equity and Inclusion lead in her division and has a special interest in improving healthcare access in the underserved population. Her research interest is in identifying causes and addressing disparities in access to kidney transplant. She is currently working with the National Kidney Foundation to improve access to kidney transplant for all thru advocacy and education of patients and kidney disease providers.
In addition, Dr. Ng also works to improve access to kidney transplant for those facing additional barriers including elderly patients, patients with frailty and/or cognitive impairment etc.

Jesse Schold, PhD, M.Stat., MEd
Visiting Professor in Surgery-Transplant
University of Colorado Health, Anschutz Medical Campus
jesse.schold@cuanschutz.edu
Jesse Schold, PhD, M.Stat., M.Ed. is Visiting Professor in Surgery-Transplant at the University of Colorado Health Anschutz Medical Campus. He received his undergraduate training at Emory University, two Masters degrees at North Carolina State University, and a Doctorate at the University of Florida.
Dr. Schold’s research interests include large database analyses, quality metrics for healthcare providers, health services research, disparities in access to healthcare and statistical and epidemiological methods. He has previously overseen outcomes monitoring and quality evaluation of the solid organ transplantation programs at the Cleveland Clinic and had a special interest in the development and use of report cards for evaluating the quality of transplant programs.
Dr. Schold has authored over 175 peer-reviewed scientific publications with primary focus in the field of organ transplantation. He has served on numerous national committees including the SRTR Scientific Technical-Advisory Committee, the OPTN Data and COIIN Advisory Committees, the AST Kidney-Pancreas and Education Committees and as an NIH Study Section Reviewer. Dr. Schold is currently a Statistical Editor for the American Journal of Transplantation. Dr. Schold has been a Co-investigator on multiple studies from the National Institutes of Health, Health Services and Resource Administration and the Centers for Disease Control and Prevention. He has given over 100 invited national and international lectures and peer-reviewed abstract presentations at scientific conferences.

Adam J. Milam, MD, PhD
Senior Associate Consultant
Division of Cardiovascular and Thoracic Anesthesiology
Department of Anesthesiology and Perioperative Medicine
Mayo Clinic, Phoenix, AZ
Milam.Adam@mayo.edu
Adam J. Milam, M.D., Ph.D., conducts research centered on environmental determinants of health. Dr. Milam uses his training in public health, biostatistics and epidemiology to examine clinical outcomes in anesthesiology and opioid addiction. His understanding of substance use at the population level as well as the individual level enables him to develop interventions to reduce opioid use during the perioperative period. This is coupled with population-level work examining trends in opioid-involved overdose deaths and health data disparities in the classification of opioid-involved overdose deaths among African Americans.
Dr. Milam also studies how health is affected by human-made structures and surroundings, often called the built environment, and by people, groups and organizations in a community, referred to as the social environment. He has been a co-investigator on several grants examining how the built and social environments shape behavioral health outcomes among adolescent populations. He works collaboratively with national organizations and policymakers to implement policies to alter the built and social environment to reduce substance use and violence exposure among youth.

Marina Serper, MD, MS
Transplant Hepatologist and Associate Professor of Medicine (Gastroenterology)
Associate Program Director for Research, Gastroenterology Fellowship
University of Pennsylvania
marina.serper@uphs.upenn.edu
Marina Serper, MD, MS is a transplant hepatologist, an Assistant Professor of Medicine in Gastroenterology at the University of Pennsylvania Perelman School of Medicine, and Staff Physician at the Corporal Michael J Crescenz VA Medical Center in Philadelphia.
Dr. Serper’s research focuses on: 1) investigating barriers to access and high quality care for patients with liver disease, 2) designing behavioral and health-system interventions utilizing health technology to improve care delivery and outcomes in chronic liver disease and liver transplantation, 3) evaluating how health literacy, medication understanding, and cognitive function affect medication adherence, self-care and health outcomes.
Dr. Serper is a health services researcher with a Master’s Degree in Health Services and Outcomes Research from Northwestern University
Contact Us
To learn more about CHART or how to join the Consortium, please contact CHART-info@duke.edu.