Limited access to the organ transplant waitlists combined with the scarcity of the organ pool results in over 100,000 deaths annually in the United States.23
Patients from marginalized groups, including women, racial and ethnic minorities, the underinsured, geographically isolated, and those with low education or income level, have disproportionately low rates of organ transplant.1-2
Inequities in access to transplant have been long-documented. Despite efforts at reform, little progress has been made.
Lack of reliable data is a principal barrier to improving equity in access to organ transplant.
- There is currently no standard for collection of patient data prior to addition to the transplant waitlist.
- National transplant data registries of transplant include few social determinants of health, with limited reliability.
- National research networks that use electronic health record data lack the ability to capture patients during specific phases of the transplant evaluation.
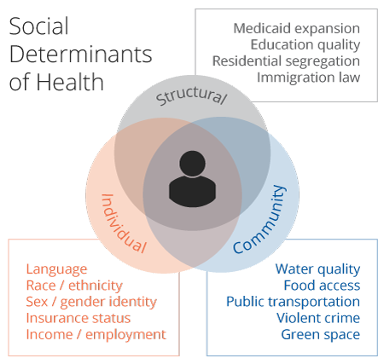
In order to effectively design interventions that improve access to transplant, there is a critical need to reliably track patients through the selection process and integrate social determinants of health data along the continuum of transplant care.
Mission
The mission of the Consortium for the Holistic Assessment of Risk in Transplant (CHART) is to impart foundational change to the process of collecting, organizing, and employing data to determine patient eligibility for transplant, leading to improved access to care, increased transparency in the transplant selection process and improved value for patients and clinicians.
Values
- Scientific rigor
- Data transparency
- Team science
Vision
Holistic transplant data collection to improve access to and outcome after transplant.
Strategic Plan
- Acquire novel multidimensional multicenter data that reflects the entire continuum of transplant care, from referral to post transplant outcomes
- Using multidimensional health system data, identify and characterize center and system level drivers of inequities in access to and outcomes after transplant
- Identify causal mechanisms between psychological risk and adverse clinical outcomes, and in doing so demonstrate the role of social determinants of health in success after organ transplant
- Identify and make accessible novel measures that improve clinicians' ability to access transplant-related risks across multiple domains and facilitate inclusive and objective risk assessment procedures
- Bring increased attention to the role of clinicians, care processes, institutional practices and reducing inequities in access to transplant and develop multilevel interventions that reduce patient vulnerability to systemic and institutional bias
- Develop and validate composite, multidimensional outcomes that reflect success after transplant
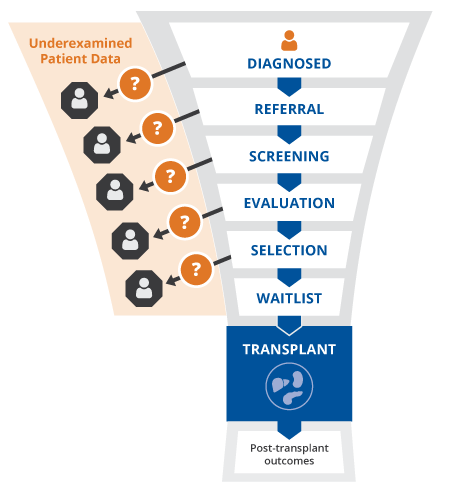
Access to organ transplant requires patients to complete a multi-phase selection process that includes collection of clinical data and data on social determinants of health.
The data on a given patient is 1) enormous, 2) located in a variety of semi-structured fields and clinical notes, and importantly, 3) not organized such that SDOH data can be integrated alongside clinical data for multidimensional risk assessment.
In the absence of accessible integrated multidimensional patient data, subjective judgments are relied upon to determine a patient’s transplant eligibility. This leaves the transplant selection process highly variable and has resulted in inequities in access to organ transplant.
Sponsors
- CareDx
- Veloxis
Contact Us
To learn more about CHART or how to join the Consortium, please contact CHART-info@duke.edu.