
National Institutes of Health grant will fund research to develop safer, more effective therapies for patients undergoing organ transplants.
Photo: Dr. Stuart Knechtle, director of the Duke Transplant Center and liver transplant specialist, and Dr. Ahmad Zaaroura, abdominal transplant fellow in surgery
Duke researchers will lead a $12 million, five-year study to test novel therapies that aim to eliminate or minimize the need for life-long immunosuppressive drugs following transplantation.
“We are extremely grateful to the National Institutes of Health for funding work that will focus on developing more effective therapies to allow transplantation in patients with immunologic barriers,” says Dr. Stuart Knechtle, Director of the Duke Transplant Center and principal investigator of the study.
For the tens of thousands of patients suffering from end-stage organ failure, organ transplantation is a lifesaving and health-extending therapy. However, transplant recipients must take some form of immunosuppression for the rest of their lives to prevent organ rejection.
Long-term immunosuppressive therapy is associated with severe side effects in transplant recipients, including cardiovascular disease, infection, and cancer. These drawbacks have driven the search for therapies that create a “tolerant” immunological state in which the patient’s immune system accepts a donor organ without mounting an immune response against the graft, known as immune tolerance.
In this study, Dr. Knechtle and colleagues will assess the role of depletional therapy as a strategy to induce immune tolerance following organ transplantation.
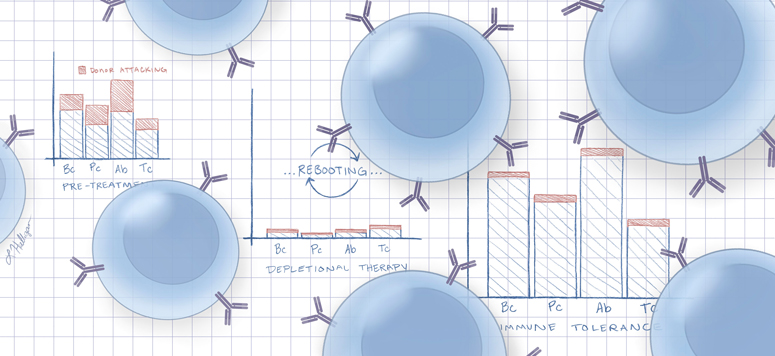
Depletional therapy conditions a patient’s immune system for transplant by wiping out B cells and antibodies, essentially rebooting the immune system to provide a welcoming, nonreactive environment for a donor organ. Currently, depletional therapy is used in over 60% of kidney transplants in the U.S. to reduce the risk of rejection, which is greatest at the time of transplant.
Dr. Knechtle and colleagues hypothesize that a patient’s response to depletional therapy depends on their immune repertoire, or the makeup of their immune system based on previous exposure to viruses and any pre-existing autoimmunity. Therefore, the effectiveness of this therapy varies from patient to patient.
In this study, the researchers will assess novel depletional therapies in a non-human primate model of kidney transplantation. The first part of the study will focus on understanding the impact of depletional induction on immune reconstitution following transplantation and how induction therapy influences the immune repertoire.
The second part of the study will focus on defining the effect of depletional therapy on the immune repertoire in sensitized transplant recipients, or recipients with antibodies that may attack a donor organ. Using desensitization therapies, the researchers aim to prep the immune repertoire to recognize the transplanted organ as one of its own.
The researchers hope that the study findings will lead to improved therapies for patients undergoing organ transplants with the ultimate goal of phasing out long-term immunosuppression from treatment protocols.
“We have wonderful scientists at Duke who will use these funds to grow our understanding of immunity and how it can be modified to promote the health of transplant patients,” says Dr. Knechtle.