
Cutting Through the Fog: One Patient’s 6-Year Journey to Finding Treatment for Primary Hyperparathyroidism
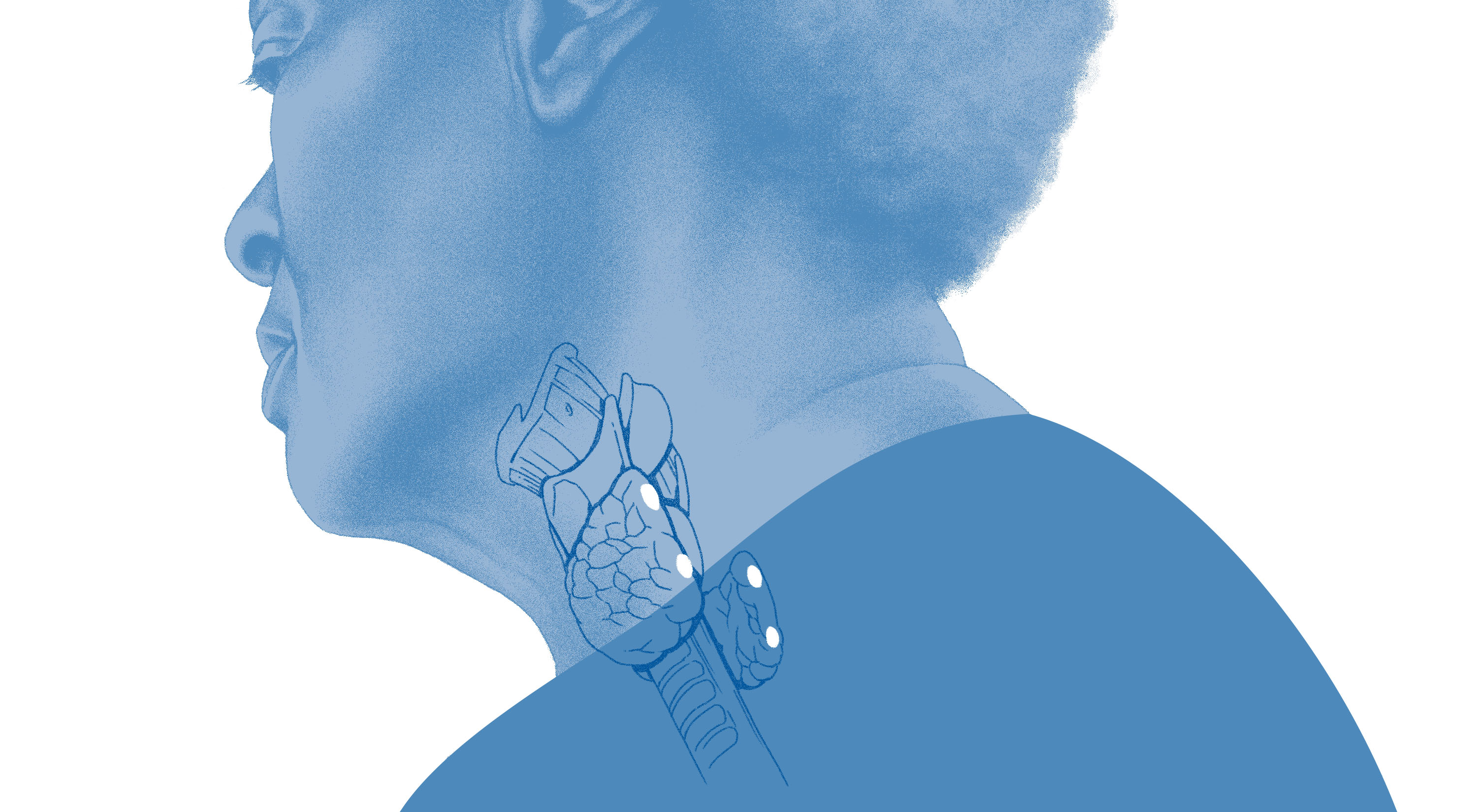
Photo above: Duke endocrine surgeon and Assistant Professor of Surgery Hadiza Kazaure, MD leads the care team to perform surgery to correct primary hyperthyroidism. Photo by Colin Huth | HuthPhoto
Six years ago, patient Patricia Bowles Carroll noticed some startling changes to her health. What began as general mental fogginess soon escalated to physical exhaustion and confusion. She realized there was a serious problem when she couldn’t make her bed in the morning without stopping to rest three times on each side.
“The symptoms were very vague,” Carroll says. “I said to myself, ‘This never happened before, why am I this exhausted?’ My house was cluttered because I got to the point that I had to save everything, because I couldn’t remember where I put things. I was concerned something was wrong. I knew I was getting older, but it wasn’t what I expected my aging to be like.”
Memory and comprehension problems began next. In her early 70s at the time, Carroll recalled her mother’s health at that age, which was markedly better than her own experience. The quality of her life, she says, was declining significantly.
“I had problems understanding people over the phone,” Carroll recalls. “It was almost like there was a delay in the conversation. I would laugh it off and say that something must be happening with me neurologically.”
Although she didn’t know it at the time, Carroll had developed an endocrine disorder called primary hyperparathyroidism, or PHPT. Patients with PHPT have an overactive parathyroid, releasing too much parathyroid hormone that monitors calcium in the blood. In turn, patients face a wide array of symptoms including malaise, body aches, and memory problems.
Despite her repeated efforts to get help, it would take Carroll over five years to be properly diagnosed and find an effective treatment.
Care for a Unique and Vulnerable Population
PHPT is a condition that affects more than a million patients over the age of 65 in the United States. As the U.S. general population ages, cases are more prevalent, but the condition remains significantly underdiagnosed. As Carroll described, symptoms can be “vague,” with more than 80% of patients lacking classic symptoms such as kidney stones and fractures that suggest PHPT.
“One of the heartbreaking things about parathyroid disease is just how underdiagnosed and undertreated it is, especially among older patients.”
- Hadiza Kazaure, MD, Assistant Professor of Surgery
Duke endocrine surgeon and Assistant Professor of Surgery Hadiza Kazaure, MD, has spent much of her career working with geriatric patients, and shares how the elderly patient population requires different approaches to care.

Assistant Professor of Surgery
“I’ve always been fascinated with the surgical care of older patients,” says Dr. Kazaure. “We definitely have some work to do to improve geriatric surgical care. Our older patients are a unique subpopulation; they’re very vulnerable. ‘Intangibles’ such as quality of life and function matter tremendously in their care. These, however, are non-traditional metrics in the world of surgery. We traditionally focus more on complications and mortality.”
For Carroll, it became imperative to find a cause for the condition that was taking these intangibles away. After the initial onset of her symptoms, she spent the next couple of years requesting her physicians to investigate further.
When Carroll’s primary care physician left his practice, she transferred to a group practice, and the high turnover of physicians there caused an incontinuity of care. What she heard repeatedly was that her high calcium levels—one of the only tests that consistently came back abnormal—were not of concern, and that she should focus her attention on addressing a separate medical condition: new-onset diabetes.

Fortunately, Carroll’s background as a social worker gave her the tools needed to advocate for her own care, and to continue searching to find answers.
“I’m fairly knowledgeable about medical systems,” Carroll says. “I’ve worked with providers. I’ve worked in the healthcare system, and I could not get my physicians to hear me. I said to them, ‘I’m presenting to you as someone with a master’s degree, I can speak with you intelligently, and I understand that something is going on with my body. You keep telling me that I’m diabetic.’”
Dr. Kazaure says that unfortunately, Carroll’s experience is not uncommon for patients with PHPT.
“One of the heartbreaking things about parathyroid disease is just how underdiagnosed and undertreated it is, especially among older patients. Data show that even among patients who have classic symptoms such as kidney stones and fractures, up to 70% are undertreated.”
PHPT isn’t difficult to diagnose if the physician knows what to look for. Blood tests often show high levels of calcium and parathyroid hormone (PTH), and those combined measurements are enough to diagnose PHPT.
Carroll’s physicians never checked a PTH level.
Taking Matters into Her Own Hands
Remarkably, surgical treatment for PHPT can cure the disorder in 95% of patients. The challenge, however, is educating primary care physicians to first diagnose the condition, and then refer patients for this treatment option.
“The surgery itself is minimally invasive, it’s outpatient,” says Dr. Kazaure. “It’s a surgical procedure that can make a huge difference in a patient’s life. Yet we’re doing so poorly in finding and diagnosing these patients and getting them to treatment expediently. Studies have shown that the lag time between diagnosis and treatment can be up to six years or more.”
What’s the reason for this gap between diagnosis and treatment? Dr. Kazaure says that too often, the patient’s symptoms are trivialized as a mild calcium elevation and in most undiagnosed patients, the stumbling block is that a PTH level has not been checked.
Carroll understands this well. She says her doctor’s first recommendation when she presented with her symptoms was to drink less orange juice to keep her calcium levels in check. Eventually, Carroll was referred to a local endocrinologist, but she was still told that her symptoms were related to diabetes even after she voiced concern over her calcium levels.
“I looked at Dr. Kazaure and as another person of color, I thought she would see me as a human being, and that’s all I wanted."
- Patient Patricia Bowles Carroll
At that point, she took matters into her own hands.
“This experience motivated me to look for an endocrinologist at Duke,” Carroll says. “All I wanted was for somebody to see me and to check this out.”
In searching for endocrinologists at Duke, she came across Dr. Hadiza Kazaure’s profile. As a Black woman herself, Carroll felt confident that a Black female physician would truly listen to her and hear her.
“I looked at Dr. Kazaure, and based on her education and her ability as another person of color, I thought she would see me as a human being, and that’s all I wanted,” Carroll says.
Three weeks later, Carroll traveled from her home in Virginia to Duke, where she met Dr. Kazaure, was officially diagnosed with PHPT, and was presented with surgery as a treatment option.
Surgical Treatment and Restoring Well-Being
In January of 2023, Carroll underwent surgery on her parathyroid gland, conducted by Dr. Kazaure. She was astounded at the immediate relief she felt of her symptoms.

“I was shocked when I came out of surgery,” Carroll shares. “Dr. Kazaure came to see me and asked how I felt, and asked if I had a sense of well-being. I cannot even describe it. The best I can say is the things that I used to worry about in terms of mental health, things I would brood over and worry about, it’s sort of like water off a duck’s back. The same problems are there, but I know I can deal with it.”
This immediate change in outlook is not only attributed to a correction in the calcium levels that were causing mental fog, but a sense of well-being in knowing that action was taken to address a condition that Carroll had suffered with for many years.
“You can actually tell that a patient is likely cured while still in the operating room; the PTH level drops profoundly within a few minutes,” says Dr. Kazaure. “When I called her recently, she said she really thought that her symptoms were due to old age, and she was so thankful that surgery had made a remarkable difference. And when I saw her again, it was like a totally different patient. We see that all the time.”
The Cultural Change Needed to Address PHPT
Because PHPT has an effective surgical treatment, Dr. Kazaure says the focus moving forward should be on raising awareness and developing resources to expedite diagnosis and treatment of the condition. She recently submitted a research proposal that will aid in the development of an artificial intelligence-based algorithm that would expedite the diagnosis and treatment of PHPT even when a PTH level has not been checked.
“The good news for us at Duke is that we are a high-volume center; we see a lot of patients with primary hyperparathyroidism,” says Dr. Kazaure. “Between our colleagues in endocrinology and us in endocrine surgery, we see more than 1,000 patients with parathyroid disease a year, maybe more. When you think about the data accumulated in the past couple of years, we can certainly develop a machine learning tool for the Duke Health system, and that’s something that could be potentially implementable nationwide too.”
Dr. Kazaure also hopes that her research will shed light on how PHPT negatively affects cognitive function, which has so far been understudied. PHPT alters the patient’s visuospatial memory, which impacts the ability to conduct tasks that require orientation and movement through space. This explains why Carroll had difficulty making her bed each morning.
“These potentially resolvable cognitive challenges are a big deal,” says Dr. Kazaure. “For an older patient, these challenges could lead to losing cherished driving privileges or could provoke conversations about a transition from independence to assisted living.”
Importantly, both Carroll and Dr. Kazaure agree that a cultural change is also necessary to improve care for patients with PHPT.
"Everybody doesn’t have the same access to care. Whatever your access is, you have to stand up for yourself. You have to fight for it. You know your own body.”
- Patient Patricia Bowles Carroll
Care for geriatric patients must go beyond dismissing characteristic symptoms of old age, they say. And because there are racial and gender disparities in the condition, underdiagnosis may disproportionately impact certain subpopulations.
Speaking eloquently and clearly, Carroll demonstrates that the fog has lifted and her struggle with primary hyperthyroidism is behind her. Now, she advocates for others.
“What do people do who don’t have the fortitude to fight through this and demand the care that they want?” Carroll says. “Everybody doesn’t have the same access to care, and it’s becoming more limited. Whatever your access is, you have to stand up for yourself. You have to fight for it. You know your own body.”