
How can a surgical program define and measure growth? The number of incoming patients? Surgical outcomes? Or is it the perioperative experience of the patient? For the section of hepatopancreatobiliary (HPB) surgery in the Division of Surgical Oncology, program growth is considered secondary to their main goal: improving overall patient care.
Focusing on all conditions of the pancreas, liver, and biliary system, HPB surgery programs are limited to highly specialized centers because of their surgical complexities. Duke is one of those centers.
A Delicate Balance
The HPB surgery program at Duke maintains a delicate balance of time between clinical and research interests. The Section of Surgical Disciplines supports faculty in maintaining this balance, allowing surgeons to research new or improved methods of treating patients.
Peter Allen, MD, Michael Lidsky, MD, and Sabino Zani Jr., MD, are passionate about improving the overall perioperative experience, especially outcomes. The team has introduced two treatments to the HPB surgical program that focus on better ways to treat patients: the hepatic artery infusion (HAI) pump and robotic liver surgery.
Implementation and growth of the HAI and robotic liver surgery programs have been possible thanks to the support and advocacy of Dr. Allen, who assumed the role of Chief of the Division of Surgical Oncology in 2018. Prior to him, Theodore Pappas, MD, was the Chief of Surgical Oncology who helped build the foundation of the HPB section. Dr. Allen’s approach has been growing the HPM section through improving services and treatment of patients.
“The goal is not growth so much as it is to deliver these programs and treatments to our patients, therefore benefitting the entire community,” says Dr. Allen. “Because of Duke’s history and legacy, we are in a great position to continue to build and deliver new therapies to our patients.”
Adjunct Therapy
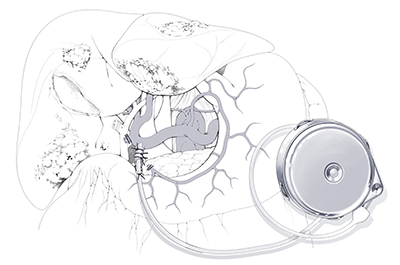
HAI surgery involves placing a subcutaneous pump and a catheter that traverses the abdominal wall and is then inserted into the arterial system of the liver via the gastroduodenal artery. HAI therapy treats cancer by delivering extremely high doses of chemotherapy directly to tumors within the liver through the hepatic artery. The most common application of HAI is as an adjunct therapy for colorectal cancer, in addition to standard chemotherapy, as a means of treating unresectable metastases in the liver.
Many patients with unresectable metastatic colon and rectal cancer are referred to Duke. Often, a local oncologist tells them that they have no other options beyond chemotherapy for the rest of their lives. For some patients, HAI is an option.
"HAI is associated with an improvement in survival, which is essentially doubled beyond that of standard therapies alone."
-Michael Lidsky, MD
Dr. Lidsky, Assistant Professor of Surgery, understood the need for this therapy and introduced HAI therapy when he joined the program in 2018, thus bringing hope to patients with colon or rectal cancer.
HAI can be used in three general scenarios: first, patients with unresectable cancers; second, borderline resectable cancers, with the goal of reducing them to resectable status; and third, as an adjuvant HAI given after complete resection of all known cancerous tissue. In the unresectable setting, controlling the cancer, or better, reducing it enough to be resected, HAI therapy contributes to improved survival. In the adjuvant setting, HAI can delay recurrence in the liver, and potentially prevent it altogether. This translates into a survival advantage as well.
“In each of these three scenarios, HAI is associated with an improvement in survival, which is essentially doubled beyond that of standard therapies alone,” says Dr. Lidsky. Unresectable metastatic disease leaves patients with too many tumors or tumors in areas of the liver where resection is not possible. In these patients, HAI, combined with standard chemotherapy treatment, can double chances of survival. “In the other group of patients that have resectable disease,” Dr. Lidsky continues, “complete surgical resection combined with adjuvant HAI yields 10-year survival rates that are just as good as it would be at 5 years if they didn’t have the pump.”
Bringing Hope Closer
“Having HAI as a therapeutic option is a nice way to restore hope and give people more time,” says Dr. Lidsky. “The quality of life that these patients have after this operation is quite good. Most of them return to work, travel, and get back to the things that bring them joy.”
Dr. Lidsky has discussed the importance of building a multidisciplinary team to provide the best patient care possible. The HPB section also intends to include the HAI therapy in the Duke Raleigh Hospital, led by Garth Herbert, MD, and Kevin Naresh Shah, MD, which will allow patients to receive care in multiple locations.
The results of the HAI therapy have been promising. Since beginning in November 2018, the Duke team had a goal of performing 10 HAI cases in their first year, but they exceeded that and completed 20 cases. The majority of these patients have achieved control of their cancer after only 3 months of HAI combined with systemic chemotherapy, and some patients who were initially deemed unresectable have converted to resection. In 2020, the team has performed six pump operations and has started using tools, such as robotics, to make the procedure less invasive.
LEARN MORE
Chemotherapy Pump Helps People With Metastatic Liver Cancer Live Longer
A New Surgical Tool
Recent advances in technology continue to improve surgical care, and surgeons in Duke’s HPB program are utilizing a robotics liver surgery to meet their needs.
Dr. Sabino Zani Jr., Assistant Professor of Surgery, leads the robotic liver surgery program. He believed that there was a need to utilize robotics from a general surgery and surgical oncology standpoint.
“I do think that patients benefit from robotic procedures,” says Dr. Zani. “It’s a minimally invasive technique that helps patients recover quicker, with less pain, and less potential complications compared to open surgery.” The goal is for patients undergoing a minimally invasive procedure to experience a reduced hospital stay and less pain, and fewer complications.
In the operating room, there is always a chance for complications. New technology requires an understanding of the major surgical procedures and intensive training to operate the machine. Dr. Zani emphasized how vital it is for surgeons to be fully prepared to operate the robot.

At the beginning, robotic surgery was used for more basic procedures, but as Dr. Zani became more familiar with the robotic equipment, he was able to use the tool to perform more complex procedures. These include the Whipple procedure and, more currently, HAI therapy and major hepatic resections.
Minimally invasive surgeries can be done laparoscopically or robotically. Dr. Zani says, “The benefits of robotics over laparoscopic surgery are multifold. One is improved vision with the use of 3D visualization as opposed to 2D. You also have instruments that have the ability to articulate so you have more degrees of freedom at your disposal.”
Dan Blazer III, MD, Program Director for the HPB fellowship, ensures that HPB fellows are offered the chance to train to operate the robotic equipment. The team agreed it was important that the fellows are given the opportunity to experience robotic surgery so that they may use it in the future.
Technology is evolving quickly, and Dr. Zani believes that it is important that surgeons at Duke continue to understand how to safely use that technology so that their patients can benefit.
Team Effort
For any decision made in the HPB section, the surgeons do so as a team. When a patient is evaluated, they build a treatment plan catered for that specific patient.
“We all discuss things and say, well, how can we make things better? What can we do differently? Where should we be pushing the envelope and advancing?” says Dr. Zani. With respect to the use of robotics for HPB surgery, “It was a discussion based on what is the best method to treat a patient.”

Determining the best method to treat their patients requires a strong team and strong leadership.
“In the modern era, with a leader like Peter Allen, a group of surgeons with a diverse set of skills, unique therapies such as HAI, and surgical approaches including open surgery, robotic surgery, or laparoscopic surgery, we are the total package as an HPB program,” says Dr. Lidsky.
New programs and tools are just the first steps to improved patient care and—eventually—growth within the HPB section.
“The best way to not only carry out the mission, but to provide the best care to the patients in North Carolina and the surrounding states, is to really invest in quality people who will bring novel programs and quality care to patients,” says Dr. Allen. “As an organization, Duke has this mentality of continual quality improvement. Always trying to deliver better quality care to the patient and that is something that the HPB program is very much a part of.”
Next Issue: Fall 2020
Be on the lookout for Surgery's Fall 2020 issue, which will feature recent advances in Duke's world-class Section of Breast Surgery, a program that treats over 1,200 patients per year.
