
Photo: Patient Elwood Linney meets with two members of the POSH team, Dr. Mitchell Heflin and Dr. Sandhya Lagoo-Deenadayalan (Shawn Rocco, Duke Health)
How would you define a successful surgery? For many patients seeking medical care, surgery is a means to an end—a hopefully minor inconvenience that will improve their quality of life. But for some, the risk of postoperative complications or a long and painful hospital stay may present formidable challenges.
In today’s healthcare landscape, patients strive to be informed partners, active in the decision-making that leads to their treatment. Improving overall outcomes while educating patients along the way is therefore an imperative to providing superior care. Empowering patients is a tall order—one that requires a redefintion of current standards of care while striving to overhaul the perioperative surgical experience.
Out With Old Methods
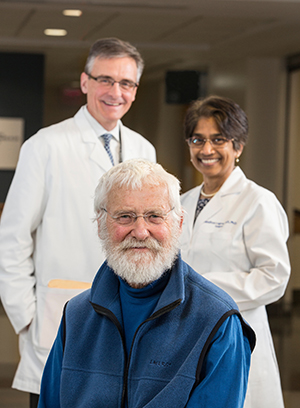
No group would benefit more from an increased focus on improving quality of care than senior patients, the population with the highest incidence of postoperative complications. The Perioperative Optimization of Senior Health (POSH) program, launched at Duke University in 2011, seeks to meet seniors’ needs.
“Nothing that we do is fancy. It is all really common sense, but it needs to be done, and it needs to be done for every patient,” says Sandhya Lagoo-Deenadayalan, MD, PhD, codirector of POSH along with Mitchell Heflin, MD, of the Department of Medicine.
Negative outcomes for senior patients can be avoidable, but only by viewing older patients as a unique subset with distinct characteristics and needs. “An older patient is different; we cannot treat them the same way that we treat a healthy 40-year-old,” Dr. Lagoo says. “Frailty, problems with nutrition, lack of physical activity, cognitive problems, management of chronic diseases, polypharmacy, social and financial vulnerability—these are all issues that need to be understood and addressed.”
POSH’s preemptive strategy anticipates potential obstacles through an interdisciplinary model of care. Eligible patients include all individuals over age 85, and those over age 65 with certain conditions, referred by surgeons to the POSH clinic for a comprehensive preoperative evaluation. Usually a few weeks before surgery, members of the surgical team, geriatricians, anesthesiologists, and social workers engage with the patient and their family in an open dialogue.
“The perioperative plan includes detailed strategies for each patient to work on before surgery, key information and recommendations for the hospital stay, and a better understanding of what transpires during recovery and transition out of the hospital,” Dr. Lagoo says. “This includes preoperative interventions to increase mobility, optimize nutrition, reduce inappropriate medications, and to flag patients at high risk for postoperative delirium.”
By meeting the entire team over a longer session, the patient has a better opportunity to understand their own goals and voice them, and for the surgical team to evaluate and address any potential roadblocks to recovery.
As of January 2018, the POSH clinic has evaluated nearly 1,500 patients. The initial results, published in JAMA Surgery in January 2018 by Dr. Shelley McDonald et al., showed that despite POSH patients being older and having more chronic conditions compared with a control group, their length of hospital stay decreased from 6 to 4 days, they had lower readmission rates at 7 and 30 days, they were more likely to be discharged to home with self-care, and they experienced fewer complications.
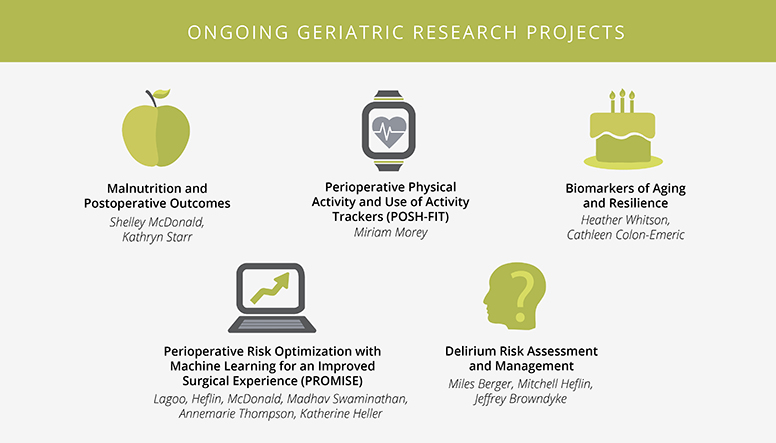
While these results are promising, Dr. Heflin and Dr. Lagoo emphasize that continued research and innovation are essential to improving care for senior patients. The team is working on developing a tool for early risk stratification of patients undergoing elective surgery. Ideally, this tool would identify surgical risk based on health factors and surgical complexity, allow for accurate triage to appropriate preoperative services, and provide early estimates of the intensity and timing of ideal optimization strategies.
POSH speaks to the power patients have over their own recovery when given the necessary tools.
New Approach to Recovery
Using a similar approach, Enhanced Recovery after Surgery (ERAS) helps patients of all ages learn new ways to accelerate their recovery. Duke colorectal surgeon Julie Thacker, MD, leads the charge at Duke in an international effort to improve outcomes.
“Currently, Duke has Enhanced Recovery pathways in place for colorectal and hepatopancreatic surgery, gynecologic oncology, renal transplant, and plastic free flap,” says Dr. Thacker. “We work to optimize outcomes and are at the forefront of protocol creation and implementation. Our work has been used as the model for a nationwide implementation program through NSQIP [National Surgical Quality Improvement Program] and the American College of Surgeons.”
"Our work has been used as the model for a nationwide implementation program."
–Dr. Julie Thacker, on ERAS
Since its inception in 2010, ERAS principles have reduced length of stay, readmission, reoperations, complications, and infections. ERAS also discourages the use of opioids, decreasing the risk of postoperative dependency. In more than half of the selected colectomy ERAS cases, the patient is discharged one day
after surgery.
Keeping the patient involved and engaged in their own recovery is an important part of the process, Dr. Thacker says. The approach begins with a discussion between the patient and a member of the healthcare team, reviewing the surgery and expectations. Combined with better nutrition before surgery, non-narcotic pain medications, and an encouragement to walk and ingest solid food after surgery, the objectives help the patient to get back to a normal routine—and back home—as soon as possible.
Duke’s ERAS model has seen nationwide implementation through NSQIP and the American College of Surgeons, and in an ongoing implementation project led by the Agency for Healthcare Research and Quality.
New Focus, Old Idea
An essential component of influencing patient outcomes is data, and lots of it; data provide the necessary benchmarks needed for improvement. According to Chief of Abdominal Transplant Surgery Debra Sudan, MD, data collection in transplant surgery is critical, but currently unstandardized and underutilized.
“Patients want to know more information before a transplant,” says Dr. Sudan. “Will they need to come back to the hospital? Are they going to need more surgeries? Will they get an infection? To some patients, this is just as important to them as living. They want to know what is expected.”
Most hospitals do not collect enough transplant surgery data to provide answers, but this may soon change with the Transplant Quality Improvement Program (TransQIP), initiated by the American College of Surgeons and the American Society of Transplant Surgeons.
If the name looks familiar, it should—TransQIP is modeled after NSQIP, an invaluable resource used by over 600 participating hospitals since 1994. NSQIP provides improvement benchmarks, but there has not been a program that provides similar transplant-specific data, until now.
"Duke supports this initiative because in the end, we are doing it to benefit our patients."
–Dr. Debra Sudan, on TransQIP
“Even though we are blessed with a lot of data collection through SRTR [the Scientific Registry of Transplant Recipients] and UNOS [the United Network for Organ Sharing] for looking at patient graft survival, the data do not look at the complications after transplant,” says Dr. Sudan. “We have been without good benchmark data for standard UTIs, pneumonia, deep vein thrombosis—and we also don’t know rates of rejection with really good validity.”
Without these benchmarks, a program has no way of knowing how it compares to other centers or where it needs to improve. TransQIP can provide answers by tracking data from both donors and recipients for one year posttransplant, helping centers to spend their time improving in the most impactful areas.
Currently, TransQIP tracks any adult patients who have a standard single-organ kidney or liver transplant in participating centers. Beginning in 8 medical centers over a 6-month alpha phase, the beta phase has expanded to 29, with a focus on learning the most important data to collect and how to report it in a
meaningful way. The next step is to follow NSQIP’s model of becoming a national standard for surgical data.
“I’m really pleased that Duke supports this initiative, as it isn’t externally funded,” Dr. Sudan says. “The hospital has committed to the cost of the extra staffing it requires for data collection—because we know that in the end we are doing it to benefit our patients.”
As TransQIP expands, it hopes to capture metrics from pretransplant data, allowing for the creation of a transplant risk calculator and decision-making tools. In this way, TransQIP data can provide key information to all stakeholders, offering answers to patients who are weighing the benefits of undergoing transplant surgery.
A New Paradigm
The surgeon, the patient, their loved ones—all may begin the surgical journey with different expectations, goals, and definitions of success. Improving outcomes is most attainable when these goals are voiced and aligned, and when the surgeon–patient relationship is viewed as a partnership by all invested in the patient’s recovery.