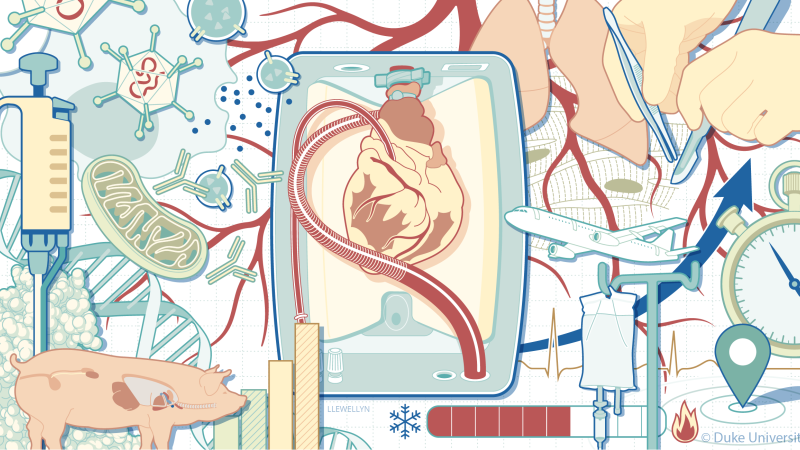
Expanding the Donor Pool in Transplantation
Optimizing Patient Options
From deep biological insights to innovative therapeutic strategies, Duke Surgery consistently expands the limits of what is possible for patient care through a culture of multidisciplinary collaboration.
In transplantation, our robust participation in clinical trials for ex vivo perfusion devices and donation after circulatory death organ utilization has impactfully expanded the donor pool for adult and pediatric patients alike, while explorations in gene therapy aim to optimize organs that would otherwise be unviable or at risk for rejection.
In this specialty and beyond, our interdisciplinary collaborations generate groundbreaking options that make our surgical care a source of hope for even the sickest patients in our care.
Advancing Novel Technologies • Restoring Viability to Organs After Cardiac Death • Adapting to Meet Complex Needs • A Platform for Future Development • Staying at the Forefront of Greatness
Advancing Novel Technologies
The Duke Department of Surgery has long been a national leader in transplantation and clinical trials that help to bring innovative technologies to market and provide new options for patients in need.
In the cardiac specialty, Carmelo Milano, MD, Chief of the Division of Cardiovascular and Thoracic (CT) Surgery, has led numerous studies to advance ventricular assist devices and total artificial heart technologies as vital options for patients waiting for a transplant. In transplantation more broadly, trials led by Drs. Milano, Jacob Schroder, Matthew Hartwig, and Andrew Barbas are further exploring the value of ex vivo perfusion devices, a rapidly growing area of innovation that is transforming the transplantation landscape.
At their simplest, ex vivo perfusion devices significantly reduce injury to donor organs by restoring circulation immediately after procurement and throughout transportation to the recipient.
"There is a lot of ischemic injury to the liver during that period of storage and transportation. So, this technology allows us to avoid that injury and transplant the organs safely to the recipient.”
- Andrew Barbas, MD
Now, what Duke surgeon–scientists are investigating further is how these devices can also be used as tools to support organs that would otherwise be unusable, assess functionality and viability of the donor organs, or even deliver targeted therapeutic medicines to further improve the recipient’s outcomes.
Combined, these advancements are ultimately leading to a larger donor organ pool and more options for transplant candidates.

Associate Professor of Surgery, Division of Abdominal Transplant Surgery
“These technologies are allowing us to transplant more livers, particularly higher risk livers, that we wouldn’t have considered usable without the technology,” says Andrew Barbas, MD, Associate Professor of Surgery in the Division of Abdominal Transplant Surgery. Dr. Barbas is also co-principal investigator of the Duke Ex-Vivo Organ Laboratory along with Matthew Hartwig, MD, Professor of Surgery in the Division of CT Surgery.
“Fatty livers or livers with advanced age or other high-risk categories, for example, don’t do well when stored on ice,” Dr. Barbas explains. “There is a lot of ischemic injury to the liver during that period of storage and transportation. So, this technology allows us to avoid that injury and transplant the organs safely to the recipient.”
In 2023 alone, Duke transplanted 165 livers, its highest annual liver transplant volume to date, thanks in part to ex vivo perfusion devices expanding the boundaries of what constitutes a viable donor organ.
Restoring Viability to Organs After Cardiac Death
Duke Surgery’s work with ex vivo perfusion technologies is also expanding the possibilities for organs donated after cardiac death (DCD).
“DCD is a category that is growing the most in our program, and now makes up about 40% of our liver transplant volume, when just a few years ago it was about 10% or less,” says Dr. Barbas. “Given the nature of cardiac death, DCD organs have some upfront ischemic injury prior to their recovery, so they historically have had worse outcomes than organs that have been donated after brain death (DBD), which have full blood flow up until the point of being removed.”
However, by restoring blood flow to these organs quickly at the donor site using ex vivo perfusion, that damage can be heavily mitigated.
"Until recently, brain-dead donors were the only donors for heart transplantation..."
- Jacob Schroder, MD, et al.
Jeffrey Keenan, MD, Assistant Professor of Surgery in the Division of CT Surgery, agrees that ex vivo interventions have been essential for expanding the cardiovascular organ donor pool.

Assistant Professor of Surgery, Division of Cardiovascular and Thoracic Surgery
“Ex vivo perfusion devices allow us to use organs that previously couldn’t be used, particularly in DCD and also in high-risk brain-dead donors,” says Dr. Keenan, “and we can travel further to procure organs than we could in the past, so we’re really using these technologies to our advantage.”
Dr. Barbas adds that prior to the development of ex vivo perfusion devices, DCD heart transplantation, specifically, wasn’t as much of a possibility.
“Until recently, brain-dead donors were the only donors for heart transplantation because brain death permitted in-situ assessment of the viability and function of the heart…before surgical procurement,” explains a team led by Jacob Schroder, MD, Assistant Professor of Surgery in the Division of CT Surgery, in a 2023 New England Journal of Medicine report demonstrating comparable outcomes between DCD and DBD hearts as a direct result of the advancements of ex vivo perfusion technology.
The ability to reanimate, evaluate, and transport DCD hearts on these devices has opened an entirely new channel of donor hearts, that is projected to expand the donor pool by 30% and substantially reduce wait times for both adult and pediatric patients alike.
Adapting to Meet Complex Needs
“No other pediatric program east of the Mississippi is doing DCD heart procurements,” notes Douglas Overbey, MD, Assistant Professor of Surgery in the Division of CT Surgery. “The problem is that we don't have pediatric-sized ex vivo perfusion systems that can let us reanimate the heart in a way that we can then prove that it's going to be functioning well before we put it in a recipient.”

Assistant Professor of Surgery, Division of Cardiovascular and Thoracic Surgery
Therefore, utilization of pediatric DCD hearts has required another innovative approach called normothermic regional perfusion (NRP) to test the heart’s suitability for transplant.
“This is something that we are leading the nation and world in,” says Dr. Overbey. “NRP can help increase the donor pool because these organs would otherwise not be used. Further, when we started using NRP as an option, our waitlist times decreased from 120 days to 33 days.”
This expansion of viable donor organs and the corresponding decrease in wait times are especially impactful for pediatric patients.
“The great part about pediatric heart transplants is that they last a lot longer and they’re immune privileged organs, as opposed to adult transplants, and the organs can last 20 years,” says Dr. Overbey, who is currently one of four congenital heart surgeons at Duke.
The downside, he explains, is that, “A three-day-old child has a radically different sized heart than a six-year-old or a 12-year-old, so the organs have to be size matched within a certain range to fit, which just also means that wait times are a lot longer than we see in adults.”
Additionally, these advancements in evaluation methodology have opened another revolutionary path for organ utilization: partial heart transplantation.
“Anything that increases our ability to conduct organ transplants also increases our ability to do partial transplants,” explains Dr. Overbey.
If a DCD heart, for example, was struggling to regain muscular strength during the evaluation stage but its valves were otherwise working properly, it previously would have been deemed unusable in its entirety. Now, thanks to the pioneering work of Joseph Turek, MD, PhD, MBA, Professor of Surgery in the Division of CT Surgery, and his team, the valvular halves of these hearts are being utilized to fix a range of congenital anomalies, substantially increasing organ availability and further reducing wait times for these pediatric patients.
Much of our ability to develop advancements in adult and pediatric cardiac care nearly simultaneously can be attributed to influential medical campus geography.
It is rare that a children’s hospital shares walls with its adult counterpart, but the close physical proximity between the adult and pediatric cardiac units of Duke University Hospital (DUH) and Duke Children’s Hospital has proven advantageous, providing better avenues (literally and figuratively) for the pediatric and adult teams to collaborate and stay on the cutting edge of mechanical circulatory support (MCS).

“Being able to work so closely with our adult cardiac colleagues means that we have access to the same tools they do, and we can use those devices such as the Impella 5.5,”—a durable implantable catheter-based MCS device that can support patients for up to months at a time while waiting for a transplant—“for larger children and adolescents, whereas otherwise we might not have familiarity with them,” says Dr. Overbey. “So, having access to those means that we’ve implanted a lot more of those types of devices than most other institutions have.”
A Platform for Future Development
Collaborations between Duke clinicians and surgical scientists are also expanding the utility of ex vivo systems as effective research platforms for studying the effects of procurement on organs and identifying therapeutic strategies that could improve the organ’s viability both in transit and in the recipients longer term.
“We started with small animal models...to establish the concept: If you deliver gene therapy to the organ and then transplant it, what are you going to see?”
- Andrew Barbas, MD
Examining the effects of procurement on a molecular, histologic, and microscopic level to evaluate why a heart donated after circulatory death might experience more injury than its DBD counterpart is one of many research projects utilizing ex vivo perfusion systems.
“We want to understand what may be happening to the heart through the course of retrieval, restoring blood flow, and implant into the recipient, so that we can have some ideas about ways that we can minimize the damage that the heart experiences,” says Dr. Keenan, who succeeded Dr. Milano as the new Surgical Director for MCS within the Duke Heart Center this year.
“Heart transplant is an amazing therapy, but the major short-term complication that we worry about is primary graft dysfunction,” he adds.
Primary graft dysfunction accounts for a majority of the short-term risk of mortality after heart transplant, and Dr. Keenan is hoping to identify pathways to reduce its risk of incidence and opportunities to deliver intervening therapeutics while the donor heart is on the ex vivo perfusion device.
As for what those intervening therapeutics might be and how they might make it into the targeted organs, Duke clinicians look to the expertise within the Division of Surgical Sciences.
Dawn Bowles, PhD, and Aravind Asokan, PhD, Professors in Surgery in the Division of Surgical Sciences, work extensively in gene therapy and its potential applications in transplantation, harnessing viruses as tools to deliver genetic “instructions” to targeted tissues and examining the impacts of these therapies on organ function and immune tolerance.
Together, Drs. Bowles and Asokan, alongside transplant surgeons Drs. Milano, Hartwig, and Barbas, are examining how the ex vivo perfusion platform’s ability to isolate an organ can facilitate delivery of therapeutics in more targeted ways than would previously have been possible. Doing so, they surmise, would both further expand the volume of transplantable organs, and mitigate recipients’ risk of rejection.
“We started with small animal models of liver and lung transplantation to establish the concept of, if you deliver gene therapy to the organ and then transplant it, what are you going to see?” says Dr. Barbas. “Down the road, our hope is to address specific genes of interest that will improve transplant outcomes and specifically reduce organ rejection rates.”
Staying at the Forefront of Greatness
A drive for innovation and an emphatic commitment to collaboration have always been at the heart of the Duke Surgery mission. As renowned leaders in transplantation, Duke surgeons and scientists are pushing the field forward in revolutionary ways, allowing Duke teams to provide care for record numbers of transplant patients.
“This is not about the work of a surgeon in isolation, it is about the rich collaborative culture that has developed within our department," says Allan D. Kirk, MD, PhD, Chair of the Department of Surgery. "The close interaction between world renown surgeons and scientists across apparently disparate disciplines is how innovation happens.”
Collaborations focused on expanding the utility of ex vivo perfusion devices, DCD organs, and genetic therapeutics are only a handful of examples, barely skimming the surface of Duke’s advancements in transplantation.
Additional in-progress studies are expanding our understanding of organ injury and rejection, and new non-human primate models of patient sensitization have identified promising treatments for this high-risk population and are effectively laying the groundwork for meaningful studies in xenotransplantation. All endeavors share the goal of optimizing the donor organ pool and improving patient outcomes.
Without Duke staying at the forefront of advancement and innovation, these successes and those to come in the future would not be possible.