But doctors seldom discuss financial differences between similarly effective treatments
Even among well-educated women with health insurance coverage, a significant proportion said the costs of cancer treatment influenced the type of surgery they chose for breast cancer treatment, a study led by the Duke Cancer Institute found.
The finding, published online in the Journal of Oncology Practice, should help guide how physicians pose treatment options to their patients, particularly as surgical approaches often have similar outcomes, but could have different costs.

“Eligible women with early-stage breast cancer often have choices for surgical treatments that are equally effective and result in excellent cancer outcomes,” said lead author Rachel Greenup, M.D., a surgeon at Duke Cancer Institute. “Surgeons often discuss the emotional and physical side-effects of treatment, yet we rarely discuss the costs.”
Greenup and colleagues conducted an electronic survey of women with stage 0-III breast cancer. The women were recruited from members of the Army of Women, a national coalition of breast cancer survivors and activists, and the Sisters Network of North Carolina, an African-American breast cancer survivors’ group.
More than 600 women participated, and their demographic profile was substantially more affluent than the U.S. average: 90% were white, 70% had private health insurance, 25% had Medicare, 78% were college educated and 56% had household incomes above $74,000 a year.
Despite such advantages, a substantial proportion of the women (43%) reported that they considered costs when making breast cancer treatment decisions, and nearly a third said cost played a role in their surgical choice. For women whose household incomes were under $45,000 a year, costs of treatment were more important than keeping their breast or its appearance -- two factors that are regularly discussed with women facing surgical choice.
Overall, 35% of respondents reported that their cancer treatment created a financial burden, and 78% never discussed costs with their cancer team. Even among participants with the highest incomes, 65% said they were fiscally unprepared for the cost of their breast cancer treatment.
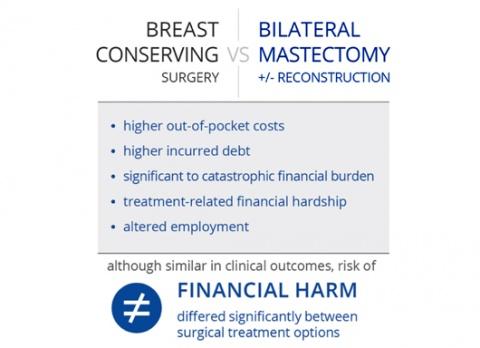
Among the procedures available for breast cancer – including breast conserving surgery (lumpectomy with radiation), mastectomy, and double mastectomy with or without breast reconstruction – double mastectomy was associated with higher patient-reported debt and financial hardship.
“Women are weighing many factors when deciding what type of surgery is best for them, including their personal desire for breast preservation, options for reconstruction, recovery
time, sexuality, appearance, demands for future surveillance, and their own peace of mind,” Greenup said.
“While other side effects of surgical choice are routinely discussed with their physicians, the potential for financial harm is not explicitly addressed, including both the out-of-pocket payments and lost productivity for patients and their families,” she said. “Our study suggests this should change.”
In addition to Greenup, study authors include Christel Rushing, Laura Fish, Brittany M. Campbell, Lisa Tolnitch, Terry Hyslop, Jeffrey Peppercorn, Stephanie B. Wheeler, S. Yousuf Zafar, Evan R. Myers and E. Shelley Hwang.
The study received support from a Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) Career Development Award from the National Institutes of Health (K12HD043446-11) and the National Cancer Institute (P30-CA014236).