Overview
Dr. Allen’s laboratory focuses on translational research in the realm of pancreatic disease and cancer. The main focus of the laboratory is in studying a cystic precursor lesion of pancreatic adenocarcinoma called Intraductal Papillary Mucinous Neoplasm (IPMN). These cysts can occur in the main pancreatic duct as well as in the branch ducts of the pancreas. These lesions may be present in as many as 10% of people over the age of 70 years and this pathway is presumed to account for 15-20% of pancreatic cancer. Study of this disease affords us the opportunity to potentially prevent pancreatic cancer, and gives us insight into the progression to pancreatic cancer.
The cause of IPMN, and the mechanisms around progression, remain poorly understood. Furthermore, the ability to differentiate between IPMN that is at low-risk and high-risk of progressing to cancer without an operation is very limited. Currently, the Allen laboratory is currently evaluating causal mechanisms of IPMN, identifying molecular markers of disease, and working with other laboratories to develop genetically engineered mouse models of this disease.
To answer these questions, the Allen laboratory has adopted several high-tech methods to detect the differences between low-risk and high-risk IPMN. These include spatial transcriptomics (NanoString GeoMx DSP, see Figure), proteomics (Olink PEA technology), and newly developed microbiome analysis methods. These novel technologies, along with the development of a murine model, allow for cutting-edge research into a disease about which little is known. Dr. Allen’s research has been funded by the NIH since 2009, and current training opportunities are available through a Surgical Oncology T32 training grant maintained at Duke for over ten years.
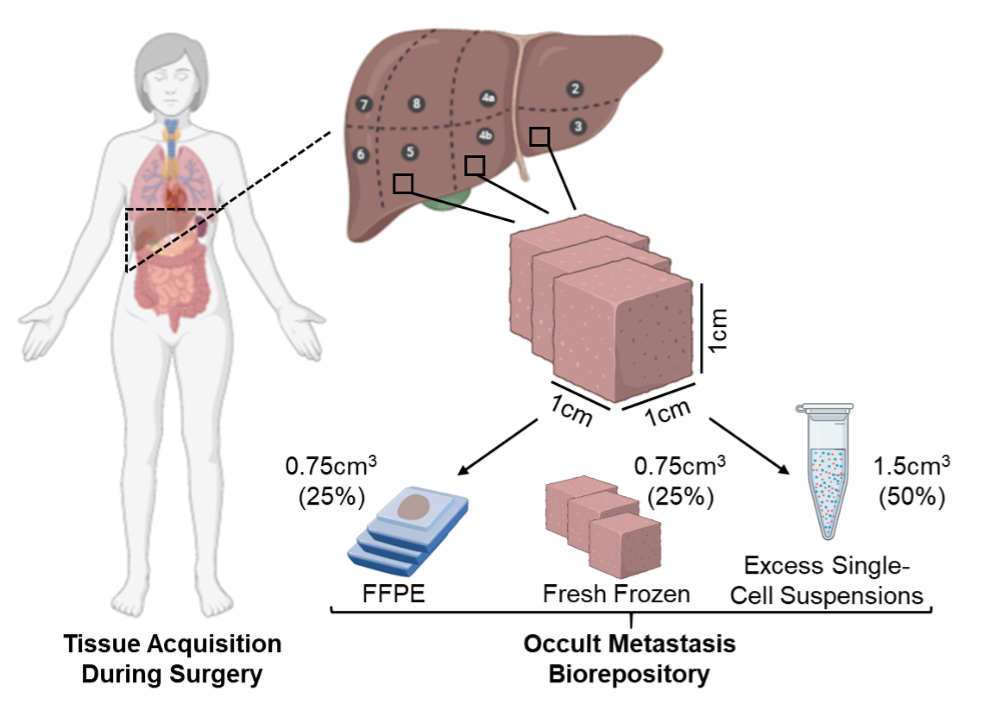
The ability to cure patients with pancreatic cancer is frequently limited by the presence of disseminated, yet radiographically undetectable (“occult”) cancer cells at the time of diagnosis. Dr. Nussbaum’s research focuses on improving our fundamental understanding of occult metastatic disease, and then developing novel strategies to prevent progression of this aggressive malignancy in order to expand truly curative treatment options. The occult nature of this disease state requires devising model systems of the earliest events in cancer cell dissemination, implementing cutting edge approaches to investigate how these cancer cells survive and proliferate in a foreign microenvironment, and ultimately translating these findings into early phase clinical trials. This “bench-to-bedside” approach is directly inspired by the pancreatic cancer patients whom Dr. Nussbaum and his colleagues treat at Duke Cancer Institute, and the commitment of the entire Hepatopancreaticobiliary Service towards improving outcomes for this recalcitrant disease.
Specifically, Dr. Nussbaum’s laboratory is focused on understanding how the hepatic microenvironment shapes the fate of occult metastatic cells, and then leveraging these findings to eradicate these cancer cells before they progress to lethal liver metastases. The rationale for this effort is that the liver is by far the most common site of metastasis for patients with pancreatic cancer (even after successful resection of their primary tumor), and that liver metastases dictate survival (even among patients with metastases to other organ sites). Upon joining the faculty at Duke University in 2021, Dr. Nussbaum developed a first of-kind, IRB-approved biorepository to obtain liver samples from patients with localized pancreatic cancer, enabling his research group to comprehensively approach this fundamental clinical obstacle. To overcome the “needle-in-a-haystack” challenge of studying ultrarare cancer cells within the vast hepatic microenvironment, Dr. Nussbaum applies spatially-sensitive and single-cell approaches not only to investigate the cell-autonomous features of these occult cancer cells, but also to explore their interactions with neighboring non-malignant cells, including hepatic immune populations. These efforts are enabled by collaborations throughout the Duke University School of Medicine, including the Center for Applied Therapeutics. Dr. Nussbaum is currently developing clinical trials for patients with localized pancreatic cancer focused on liver-directed therapy to prevent the outgrowth of hepatic occult metastatic cells. His research has previously been supported by the National Institutes of Health/National Cancer Institute, and is actively supported by the National Comprehensive Cancer Network.
Publications and Funded Projects
View Dr. Allen's profile to see his publications and funded projects.